Managing Pre-Infusion Hyperglycemia: Rapid vs. Regular Insulin
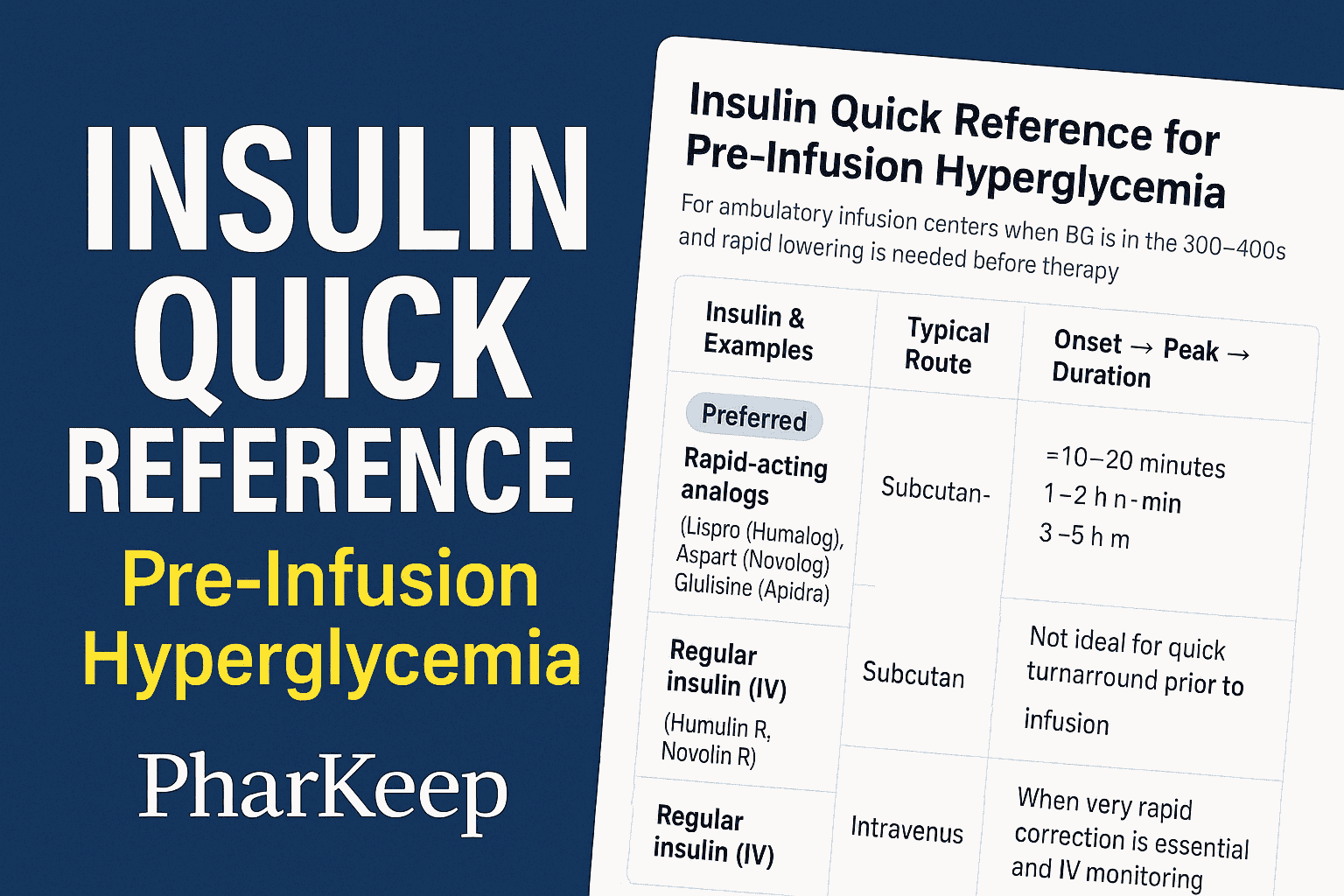
In infusion centers, rapid-acting insulin analogs are preferred for correcting blood glucose before therapy. Learn why onset, duration, and safety matter, and how to select and dose insulin for quick, effective correction.
Introduction
Pharmacists in infusion centers often encounter patients presenting with markedly elevated blood glucose—sometimes in the 400 mg/dL range—prior to receiving chemotherapy, biologics, or other infusion medications. Since hyperglycemia can increase risks during treatment, lowering blood glucose to a safe threshold is often necessary before proceeding. Choosing the appropriate insulin formulation is a critical clinical decision that directly impacts safety, timing, and patient outcomes.
Pharmacologic Profiles: Rapid-Acting vs. Regular Insulin
- Rapid-acting insulin analogs (lispro, aspart, glulisine):
Onset within 10–20 minutes, peak effect at 1–2 hours, and duration of 3–5 hours. These agents are ideal when infusion timing is constrained because they provide quick correction with less risk of prolonged hypoglycemia. - Regular insulin (subcutaneous):
Onset 30–60 minutes, peak at 2–4 hours, duration up to 8 hours. While effective for general glycemic control, its slower onset and prolonged tail make it less practical when an infusion must begin soon. - Regular insulin (intravenous):
Acts almost immediately and is the gold standard in acute inpatient settings (e.g., diabetic ketoacidosis). In outpatient infusion centers, IV insulin is rarely used due to monitoring requirements.
Clinical Application in Infusion Centers
- Preferred approach: Subcutaneous rapid-acting insulin analog for correction when blood glucose is in the 300–400s, with recheck in 60–90 minutes.
- Alternative: IV regular insulin for urgent correction if IV access and monitoring protocols are available.
- Avoid: Subcutaneous regular insulin when a timely drop in glucose is required; the onset is too slow, and the duration is unnecessarily prolonged.
Correction Dosing Considerations
- Typical correction dose: 0.05–0.1 units/kg subcutaneously (about 4–10 units in most adults).
- Use lower doses (0.03–0.05 units/kg) in frail or renally impaired patients.
- Adjust upward in patients on steroids or with significant insulin resistance.
- Always pair with a glucose recheck at 60–90 minutes before proceeding with the infusion.
Key Safety Pearls
- Rule out diabetic emergencies (DKA/HHS) before routine correction.
- Never stack insulin doses without follow-up monitoring.
- Educate patients about the possibility of delayed hypoglycemia post-discharge.
- Consider the underlying cause of hyperglycemia (missed basal insulin, infection, steroids).
Conclusion
For infusion centers, subcutaneous rapid-acting insulin analogs are the optimal choice for correcting pre-infusion hyperglycemia due to their faster onset and shorter duration. Regular insulin—especially subcutaneous—poses timing and safety challenges. Pharmacists and pharmacy learners should be prepared to recommend and monitor rapid-acting correction strategies while individualizing doses to patient characteristics.
Related Articles




